 The Supreme Court—through the actions of tie breaker Chief Judge John Roberts—has resolved the constitutionality of the Patient Protection and Affordable Care Act (ACA). In the best tradition of the court, his Solomonic ruling declares that the law is within the powers of Congress. Good law? Bad law? “Not my problem. It’s constitutional.” He also applied the “duck” test to the Administration’s “penalty”—if it looks like a tax and quacks like a tax, it’s a tax.
The Supreme Court—through the actions of tie breaker Chief Judge John Roberts—has resolved the constitutionality of the Patient Protection and Affordable Care Act (ACA). In the best tradition of the court, his Solomonic ruling declares that the law is within the powers of Congress. Good law? Bad law? “Not my problem. It’s constitutional.” He also applied the “duck” test to the Administration’s “penalty”—if it looks like a tax and quacks like a tax, it’s a tax.
The constitutional sideshow behind us, let’s get back to the Main Event: Health care remains an unaffordable, inequitable mess. ACA addresses some of the coverage problems built into the American health insurance model, but it will inevitably create some inequities of its own.
Cost is still an enormous problem. In fact, the law will increase the share of GDP spent on health care. ACA’s supporters are eager to report the Congressional Budget Office (CBO) finding that the law will not increase the deficit. First, remember that this is a forecast built on complex models, loaded with assumptions. The CBO finding is an estimate, not a measurement.
More importantly, the much-quoted finding is about the nation’s deficit, not the cost of the law. You’ve bought a new car, but a second job covers the payments. At the end of the month you’ll have the same amount of cash left over as before, but the car isn’t free. Increasing health insurance coverage for millions of Americans won’t be cheap. That same CBO estimates that the gross cost from 2012—22 will be $1.8 trillion (http://goo.gl/oFZW5).
Act II needs to be about cost. Yes, some provisions in ACA address the cost problem, but these are baby steps. The Rochester area has played a role in cost control in the past and is taking steps to continue to serve as a national role model.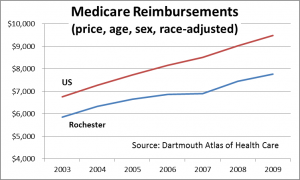
The Dartmouth Atlas reports that the total cost per Medicare recipient in the Rochester Hospital Referral Region (HRR) was nearly 20% lower than the nation (when adjusted for price, age, sex and race). Medicare principally cares for the elderly.
Lower cost also applies to health care for Rochester’s non-elderly population. A study of commercial insurance conducted by the Milliman consultancy reported that for 2007, insurance cost per member per month in Rochester was almost ¼ lower than the nation.
The critical question, of course, is why is health care cheaper in Rochester? Dartmouth’s analysis indicates that physician spending for Medicare patients is much lower in Rochester, 74% of the national average. For the non-elderly addressed by the Milliman study, the lowest cost category is inpatient hospital care—63% of the comparable cost for the nation.
Lower cost=higher coverage? Is it surprising that the share of the Rochester population without health insurance is also lower? Of New York’s largest 15 counties, only Staten Island has a lower uninsured rate than Monroe County. That’s a concern about ACA, incidentally. By driving up the cost of health insurance, ACA is likely to push more people into the public insurance pools.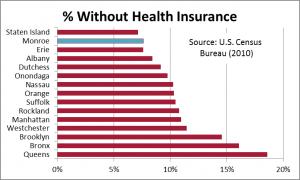
The researchers at Dartmouth believe that excess capacity drives up cost. Beginning 50 years ago, business leaders and the Finger Lakes Health Systems Agency tightly managed hospital expansion. By limiting capacity, Rochester kept cost in check. As the Milliman data suggest, the cost impact of capacity control continues to this day. It is not an accident that when the NYS Commission on Health Care Facilities in the 21st Century (the “Berger Commission”) targeted excess health facilities for closure, Rochester was conspicuous by its absence.
Controls over the purchase of capital equipment have had a similar effect. The Community Technology Assessment Advisory Board (CTAAB), established in 1993, reviews requests for new capital equipment. If CTAAB believes that the additional equipment isn’t needed, the insurers generally don’t reimburse for its use. Nowhere is this more evident than in the MRI utilization rate—the rate for the Finger Lakes is well below that of the state and nation.
Recently released results of the Rochester Medical Home Initiative, a new approach to primary care administered by Excellus and MVP, prove that vigilant primary care can reduce overall system cost. Participants in the trial reduced overall cost by trimming unnecessary hospital admissions, re-admissions and use of hospital emergency departments. It is this trial that will be dramatically expanded under the $26.5 million awarded to the Finger Lakes Health Systems Agency by the Federal Center for Medicare & Medicaid Innovation (CMMI) grant program. The grant is for providing a more comprehensive primary-care model to patients at high risk for hospitalizations and emergency-room visits.
Most experts agree that much of health care spending is unnecessary—or even harmful. The quip is that “Half of all health spending is wasted—we just don’t know which half.” A consortium of Rochester health care providers, business leaders, and insurers are seeking support to bring clinical data together to figure this out. The Finger Lakes Regional Clinical Quality Improvement Initiative is intended to identify what works, what doesn’t, and to disseminate this information to physicians throughout the region.
The high and rising cost of health care is among the most significant problems confronting our nation. There are no easy solutions to the problems of coverage and cost. Rochester is again on the frontier, however, demonstrating that broad coverage, high quality and manageable cost can go together.