 By all accounts, the Affordable Care Act’s front door, healthcare.gov, performed admirably for consumers in its second year (although “back end” problems remain). Just to keep track, I registered on the site and have been getting a steady stream of emails and text messages ever since—29 text messages since October 24! They are filled with teasers like, “8 in 10 people who sign up can get financial help. You could too!” plus special messages for special days: “Cyber Monday: Shop for health plans today” and “Start the New Year with new health coverage.” And plenty of countdowns: “Only 9 days until the Dec 15 deadline” and, on Sunday, “Act now: Only hours left! This is your last chance to enroll . . .” Except that if you claim to have tried by Sunday, you’ll have until 2/22 to sign up for March 1 coverage. And the deadline to avoid an income tax penalty will likely be extended right up to Tax Day, avoiding shock and horror when the penalty becomes real.
By all accounts, the Affordable Care Act’s front door, healthcare.gov, performed admirably for consumers in its second year (although “back end” problems remain). Just to keep track, I registered on the site and have been getting a steady stream of emails and text messages ever since—29 text messages since October 24! They are filled with teasers like, “8 in 10 people who sign up can get financial help. You could too!” plus special messages for special days: “Cyber Monday: Shop for health plans today” and “Start the New Year with new health coverage.” And plenty of countdowns: “Only 9 days until the Dec 15 deadline” and, on Sunday, “Act now: Only hours left! This is your last chance to enroll . . .” Except that if you claim to have tried by Sunday, you’ll have until 2/22 to sign up for March 1 coverage. And the deadline to avoid an income tax penalty will likely be extended right up to Tax Day, avoiding shock and horror when the penalty becomes real.
Final enrollment figures will be forthcoming, but the Congressional Budget Office recently estimated that enrollment through the exchanges (both federal and state-run) will hit about 12 million this year (the White House reported 11.4 m by the deadline). CBO’s figures indicate that the Affordable Care Act has spurred an additional 11 million Medicaid enrollments, while reducing enrollment through other channels by about 5 million. The net increase in the number of individuals with health insurance as a consequence of the law totals about 19 million.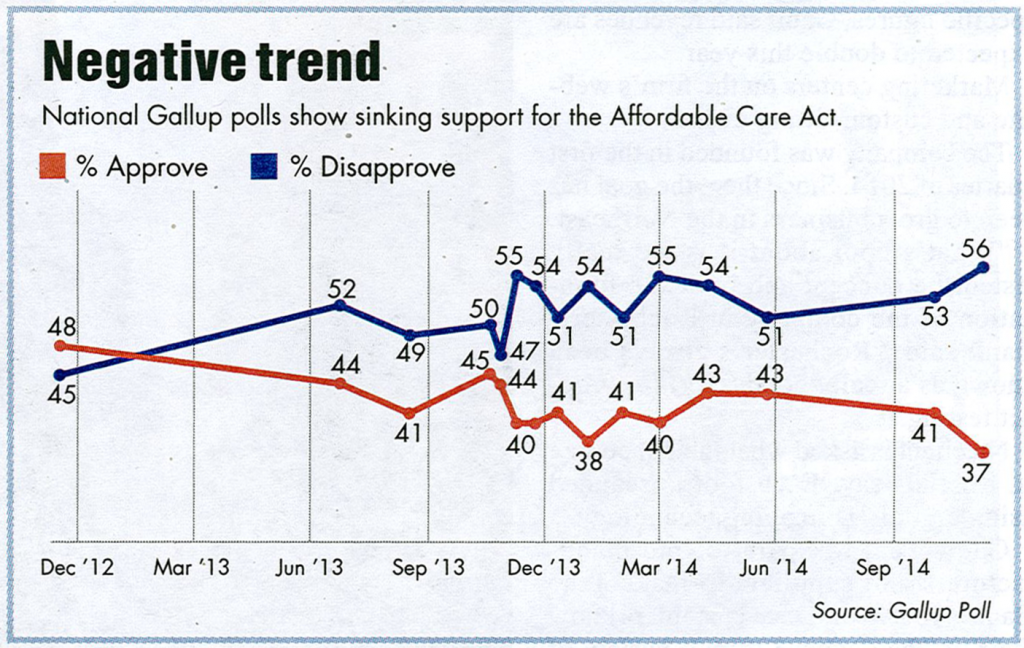
The political dynamic is fascinating (if you enjoy this sort of thing). Remember the old saw, that voters “hate Congress but love their Congressman?” ACA suffers from the schizophrenia. In November, Gallup reported that only 37% of the American public approve of ACA and 56%—a new high—disapprove. Support for specific provisions of the law—keeping dependents on family policies through age 26, eliminating the “pre-existing condition” exclusion for new policies, etc—is strong, however. Moreover, the CBO estimates that 9 million of those receiving coverage through the exchanges are getting subsidies—an average of $4,300 each. While these voters may express their disapproval of “Obamacare,” it’s a good bet that they’ll want their subsidies to continue.
As the Internet’s “Thanks, Obama” meme suggests, Obamacare is being blamed for all of the health system’s ills. A friend was told recently that her cataract surgery was being delayed because of ACA; a pharmacy employee reports that many customers complain that their drug costs have soared under the law. While the indirect effects of ACA are sweeping, neither is a direct outcome of the law.
Expansion of Medicaid coverage, one of ACA’s structural timbers, became voluntary after the Supreme Court’s NFIB v. Burwell ruling in 2012. Yet governors of refusenik states have been under pressure to expand Medicaid. Principled opposition is hard to maintain when massive federal subsidies are in the offing.
By not expanding Medicaid coverage, a “coverage gap” emerged that is manifestly unfair. A nondisabled, childless adult earning 100% of the federal poverty line ($11,770 in 2015) is eligible (obligated under the law, actually) to buy health insurance for an annual premium of 2% of income, $235, with the federal subsidy making up the difference. A loss of income—say, to $11,500—eliminates eligibility for Exchange subsidies. In the more than 20 states that didn’t expand Medicaid, nondisabled, childless adults at this income level would lose access to health insurance completely.
The Administration has been very willing to negotiate a compromise with nonexpansion states—the deal reached in a number of states, most recently Indiana, would seem to reinforce the states’ role as public policy laboratories. Indiana’s plan is worth studying, as it maintains most of the objectives of ACA but with cost-sharing and incentives that conservatives will like. For example, new enrollees in the expanded Healthy Indiana Plan (HIP) will be required to pay something toward their coverage to get full benefits—as little as $1 per month, but something. Moreover, coverage would not begin until the first premium payment is made, not on the date of application as in traditional Medicaid. Other financial incentives apply—co-payments up to $25 apply for nonemergency use of the hospital emergency room. And the benefits plan is somewhat trimmed, e.g. non-emergency medical transportation is disallowed for new enrollees.
All eyes will be back on the Supreme Court in just a couple of weeks, however. Oral argument in King v. Burwell is scheduled for March 4. Here’s the issue in the case: Whether by accident or intent, a plain language reading of the Affordable Care Act says that federal subsidies are only available to individuals who get coverage through a state-run exchange. 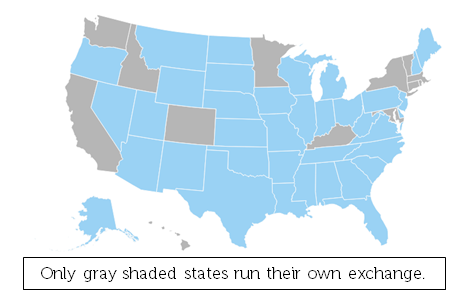 If the Court finds for the plaintiffs when it issues its ruling this summer, that could eliminate subsidies for a lot of people and put governors and legislatures in 37 states in a very awkward position. The Urban Institute estimates that 9.3 million individuals are likely to lose subsidies and that 8.2 million will lose coverage if the subsidies are ruled invalid.
If the Court finds for the plaintiffs when it issues its ruling this summer, that could eliminate subsidies for a lot of people and put governors and legislatures in 37 states in a very awkward position. The Urban Institute estimates that 9.3 million individuals are likely to lose subsidies and that 8.2 million will lose coverage if the subsidies are ruled invalid.
If you consider what we’ve learned from the Gallup Poll, many of the 9.3 million would declare their support for repealing “Obamacare.” And nearly all will also want to keep their subsidy. Ain’t politics grand!